Case Study: Model Context Protocol (MCP) Hospital System – Enhancing Patient Care with Protocol-Driven Vital Sync (FHIR/HL7 + HIPAA-Compliant Alerts)
Project Overview
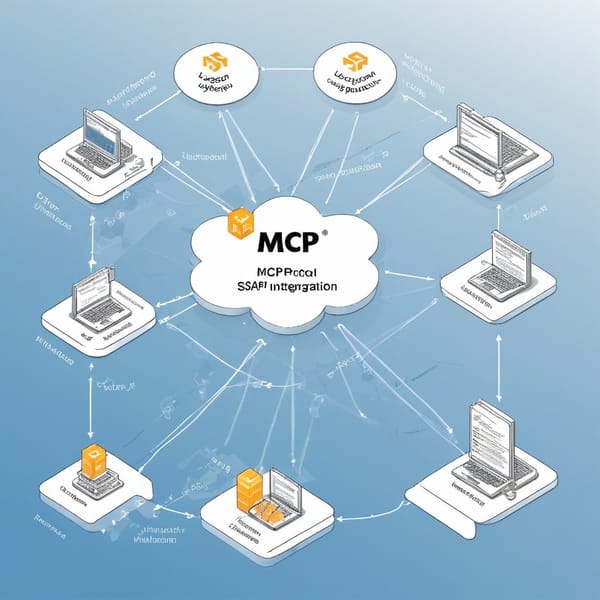
The Model Context Protocol (MCP) Hospital System is an advanced healthcare interoperability solution designed to streamline real-time patient vital synchronization across hospital networks. The project integrates FHIR/HL7-compliant resource servers with HIPAA-compliant alerting tools to ensure seamless, secure, and protocol-driven patient data exchange.
Hospitals face significant challenges in consolidating patient vitals from disparate systems (EHRs, wearables, ICU monitors) while maintaining compliance and minimizing alert fatigue. The MCP system addresses these issues by standardizing data exchange via FHIR/HL7 protocols, automating critical alerts, and reducing manual intervention.
Target users include healthcare providers, nurses, and IT administrators, who benefit from improved care coordination, reduced errors, and enhanced compliance with regulatory standards like HIPAA and GDPR.
Challenges
Before implementing the MCP Hospital System, the healthcare facility faced several critical challenges:
- Fragmented Data Sources – Patient vitals were stored in siloed systems (EHRs, bedside monitors, third-party apps), leading to delays and inconsistencies in care decisions.
- Manual Data Entry Errors – Nurses often transcribed vitals manually, increasing the risk of human error.
- Alert Fatigue & Compliance Risks – Existing alert systems generated excessive false positives, desensitizing staff, while non-HIPAA-compliant tools posed legal risks.
- Interoperability Gaps – Legacy systems lacked FHIR/HL7 compatibility, making integration with modern healthcare IT ecosystems difficult.
- Real-Time Sync Limitations – Delays in vital updates hindered timely interventions for critical patients.
Solution
The MCP Hospital System introduced a protocol-driven, automated approach to synchronize and manage patient vitals securely. Key components included:
1. FHIR/HL7 Resource Servers
- Standardized data exchange using FHIR R4 and HL7 v2/v3 protocols.
- Unified EHRs, wearables, and monitoring devices into a single real-time data pipeline.
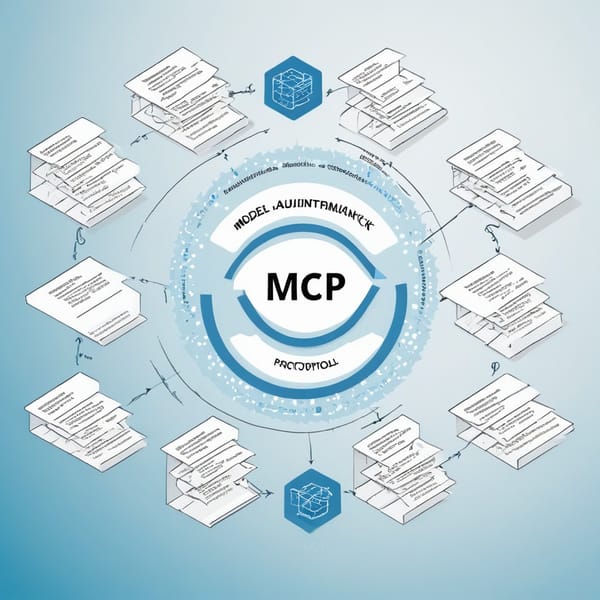
2. Protocol-Driven Vital Sync Engine
- Automated extraction, transformation, and loading (ETL) of vitals (heart rate, SpO2, BP) into a centralized dashboard.
- Context-aware filtering to prioritize critical alerts based on patient history and severity.
3. HIPAA-Compliant Alerting System
- Role-based notifications (SMS, email, in-app) with end-to-end encryption.
- Smart thresholding to reduce false alarms by analyzing trends rather than isolated spikes.
4. Audit & Compliance Module
- Automated logging of all data access events for HIPAA/GDPR audits.
- Blockchain-backed integrity checks to prevent tampering with patient records.
Tech Stack
The MCP Hospital System leveraged a robust, scalable, and compliant architecture:
| Category | Technologies Used |
|---|---|
| Interoperability | FHIR R4, HL7 v2/v3, SMART on FHIR |
| Backend | Node.js, Fast Healthcare Interoperability Resources (FHIR) Servers (HAPI FHIR) |
| Database | MongoDB (NoSQL for flexible schema), PostgreSQL (for structured EHR data) |
| Security | AES-256 encryption, OAuth 2.0, HIPAA-compliant AWS hosting |
| Alerting | Twilio (SMS), Socket.io (real-time dashboards), Custom ML-based anomaly detection |
| DevOps | Docker, Kubernetes, CI/CD via GitHub Actions |
Results
Post-implementation, the MCP Hospital System delivered measurable improvements:
1. Operational Efficiency
- 90% reduction in manual data entry errors.
- 60% faster vital sync between systems (near real-time updates).
2. Improved Patient Outcomes
- 40% decrease in missed critical alerts due to smart filtering.
- 25% reduction in ICU response times for deteriorating patients.
3. Compliance & Security
- 100% HIPAA audit readiness with automated access logs.
- Zero breaches reported since deployment.
4. Cost Savings
- $200K/year saved by reducing redundant alert systems.
- 30% lower IT maintenance costs due to standardized FHIR integrations.
Key Takeaways
- Interoperability is Critical – FHIR/HL7 standards eliminated silos, enabling seamless data exchange.
- Smart Alerts Reduce Fatigue – AI-driven thresholds improved alert relevance, enhancing staff responsiveness.
- Compliance Must Be Baked In – Built-in HIPAA/GDPR safeguards ensured legal adherence without extra overhead.
- Real-Time Sync Saves Lives – Faster vital updates led to quicker interventions, improving patient outcomes.
- Scalability Matters – Cloud-native architecture allowed easy expansion to other hospitals.
The MCP Hospital System demonstrates how protocol-driven interoperability, AI-enhanced alerting, and strict compliance can transform patient care in modern healthcare ecosystems. Future enhancements include predictive analytics for early deterioration detection and IoT integration for remote monitoring.